Child Health
At Bluff Road Medical, we offer a broad range of child health services. Our team of leading Bayside GPs are warm and compassionate – just what you want in a family doctor. Below you will find some information about common issues seen in childhood and adolescence. It is by no means exhaustive, so please reach out if you do not see what you are looking for.

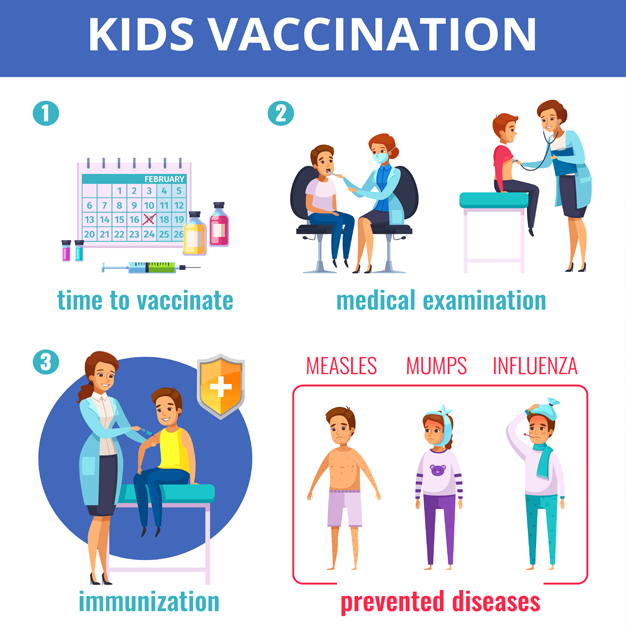
Immunisations can help protect your little ones from serious childhood infections such as meningitis, measles, hepatitis B and whooping cough to name a few. We offer vaccination sessions several times a week with our trained immunisation nurses.
Session times are: 10am – 12pm. Please call to check appointment days and availability.
Please bring your child’s My Health and Development Record (the green book) to the appointment.
The National Immunisation Program (NIP) covers routine childhood immunisations free of charge. These can be administered by a GP, our nurses or also at local council sessions.
Childhood immunisations are recommended at periodic intervals a few months apart, from birth until 4 years of age, according to the Victorian immunisation schedule. Your baby’s first vaccine is often booked at the same visit following a new mum’s six-week post-natal health check. For more information, see the Victorian Government’s Better Health page.
Most vaccinations are administered via an injection in the arm or leg. Rotavirus vaccine is given by mouth. Vaccine doses may include protection against one or several different types of infections to minimise the total number of injections given at the one visit.
Extra vaccines may be recommended in some instances and provided under the NIP, for example in babies who were premature or of low birth weight, or in children with high-risk medical conditions.
Additional vaccinations not subsidised by the Government are also available for your child. Speak to your doctor if you would like to discuss these further.
- Meningococcal B – (Bexsero) vaccine
This vaccine provides protection against the commonest form of bacterial meningitis in Australia. It is currently only provided by the government to certain groups at greater risk of infection. For most patients, this extra vaccine will need to be privately funded, further information here.
- Chicken Pox booster
One dose is currently funded and given at 18 months of age. Research shows that two doses of chickenpox vaccine provides increased protection from infection.
Some children may prefer to be vaccinated outside of the school setting and feel more comfortable with your family doctor. You can also arrange a catch-up appointment with your GP to administer any vaccine if your child misses their school vaccination session.
If your child is heading overseas on a school learning journey or family vacation, please book them in for a travel medicine consultation. The doctors can provide tailored advice about the travel vaccinations your child may require and advise on any travel risks.
While vaccines are overall extremely safe and effective, some children may experience reactions, which are usually mild and temporary. These may include a mild fever or pain at the injection site.
Meningococcal B (Bexsero), for example, may cause a fever in children under two. Speak to your doctor or our nurses about how to manage any potential side effects (for example, administering paracetamol 30 minutes before the vaccination in this instance, or using a cool compress if the injection site causes discomfort).Your child’s safety is our priority, which is why we have introduced SmartVax, a software tool to monitor adverse reactions following immunisation. Patients receive an SMS 3 days after having a vaccination at Bluff Road Medical to check on their progress and wellbeing. If there are any significant issues, your GP will be notified for follow-up.
If you are concerned about any side effects, please see your doctor, immunisation nurse or go directly to a hospital. You can also contact SAEFVIC, the Victorian vaccine safety service (call 1300 882 924 and select option 1).
Early Childhood
Developmental milestones are things most kids can do by a certain age. The way your child moves, speaks, learns and plays provides important insight into their development.
You can find information about these milestones inside your child’s My Health, Learning and Development record (‘Green Book’). Your Maternal and Child Health Service nurse will talk to you about these milestones at your regular maternal and child check-ups.
If you have any worries about your child’s development, including any speech or hearing concerns, the doctors are here to help. We have a team of GPs with specialised interests in child health who are ready to assist and if needed, refer your child to paediatric specialists or allied health professionals where necessary.
Likewise, if your baby or toddler is experiencing sleep concerns such as a sudden change in sleeping pattern or frequent night waking, this can be distressing for the family, please seek advice from us about strategies to help manage these problems.
Constipation is a very common problem in childhood. It can start as early as when your baby transitions off breast milk to start solid foods. Constipation may also coincide with a negative experience such as a painful bowel movement.
Symptoms to look out for include:
- Stomach cramps
- Loss of appetite
- Irritability
- Anal fissures (small splits of the skin around the anus) that cause pain and bleeding when going to the toilet
- Holding-on behaviour.
Please book in with a doctor if you are concerned about your child’s bowel habit. For more information about constipation management, refer to this .
Bedwetting is a common problem for young children, and it can cause sleepless nights for the family, as well as distress for the child. Daytime control usually starts to occur around the age of 4, however 1 in 3 children wet the bed. At 6 years of age, around 1 in 10 continue to do this and lessening into adolescence.If your child is still regularly wetting the bed at night by age 6, or if they suddenly start to wet the bed after six months of being dry, it may be a good time to book in and speak with your GP. This fact sheet has more information.
Treatment of enuresis takes time and may involve several health care providers including your GP, a paediatrician or psychologist (at Bayside Specialist Suites) or a continence therapist. We can also provide advice for children experiencing other continence issues such as frequency issues or giggle incontinence (involuntary urine loss when laughing).
Urinary Tract Infections (UTI) are relatively common in children, particularly in girls. A UTI occurs when bacteria enters the bladder via the urethra.
Symptoms of UTIs in babies and smaller children may include:
- Irritability
- Tiredness
- Quietness
- Disinterest in feeds
- Frequent crying
- Paleness or flushing.
In older children, symptoms may include:
- Pain or burning when urinating
- More frequent urination
- Pain in the lower tummy (or back, if the kidneys are compromised)
- Blood in the urine
- Fever
- Vomiting
If your child has a fever with no obvious cause or displays any of the above symptoms, please book in to see your GP.
Asthma is a common medical condition affecting the airways – 1 in 10 Aussie kids have asthma. It often goes hand in hand with other allergies like hay fever and eczema
A child experiences symptoms of asthma when the airways tighten as the lining of the airway becomes swollen and inflamed and this causes excess mucus production. This can cause:
- Chest tightness or pain (often described by young children as a ‘sore tummy’)
- Shortness of breath
- Difficulty breathing
- Wheezing – whistling noise when breathing out
- Coughing (particularly at night)
If you have concerns about your child’s breathing, please book in with your GP. Most children with asthma can be safely managed by your GP but we may occasionally refer you to a paediatrician or paediatric respiratory specialist for a review.
If your child does have asthma, it is important they have an Asthma Action Plan. This forms an important communication and education tool for parents and caregivers. For further reading about asthma in children, refer to the Better Health website

Symptoms of a mild or moderate reaction may include
- Rash, hives or welts
- Swelling of the face, eyes or lips
- Tingling or itchy mouth
- Eczema, hay fever or asthma – these symptoms might be worse than usual
- Mild diarrhoea, stomach pain or vomiting (if this occurs after an insect sting, it may be a severe allergic reaction).
Symptoms of anaphylaxis, or a life-threatening severe allergic reaction may include:
-
- Difficult or noisy breathing
- Tongue and throat swelling or tightness
- Difficulty talking or a hoarse voice
- A wheeze or persistent cough
- Persistent dizziness or fainting
- Paleness and floppiness (in young children)
- Diarrhoea, stomach pain or vomiting after an insect sting
If you suspect your child may have allergies, the first step is to speak to your GP.
Dr Joanne Simpson, a General Practitioner with advanced training in allergy assessment and management, is available at Bluff Road Medical to perform an allergy assessment.
If a skin prick test is required, your child will be required to attend the clinic on another occasion. You should allow 60-90 minutes for this appointment, as it will involve skin-prick testing, followed by a wait time to allow any possible reaction to develop and then a further review to interpret test results. These options will then be discussed in detail including any further management advised. Allergy tests should be avoided when your child’s asthma is unstable or if you are generally unwell.
Please fill out our allergy questionnaire prior to your consultation. To access this and further allergy information, click here.
Is your child starting school? Before the big day, it’s a good idea to arrange a general health check with your GP to ensure your child is fit and ready for this exciting new chapter.
During this appointment, your GP will run through a check list of things encompassing your child’s development including speech and behaviour, as well as habits of their bowels, bladder, or sleep.
It is worth considering getting your child’s eyes checked by an optometrist in readiness for school. We can also provide educational materials around school readiness routines, and tips for things like diet and the importance of oral hygiene.
Autism Spectrum Disorder is a developmental disorder that may affect someone’s social interactions, communication, behaviour and interactions with the world. It encompasses Asperger’s syndrome.
Sometimes symptoms can be apparent from a very early age. Other times they may not be noticeable until the ages of two or three, or even later.
Early diagnosis and treatment can lead to better outcomes for those with ASD. Some of the symptoms to look out for include:
- Lack of social or emotional exchanges like pointing and smiling
- Lack of non-verbal communication such as nodding and shaking head
- Difficulty developing friendships
- Delayed speech and understanding of speech
- Lack of eye contact
- Excessively following routines, patterns or behaviour, and becoming distressed at changes
- Repetitive play behaviour or difficulties transitioning from one play activity to another
- Sensory sensitivity to particular stimuli like sound or textures
- Restricted or fixated interests such as only playing with certain toys or talking about certain things
- Being aggressive toward others or themselves.
If your child is exhibiting any of these symptoms, please consult your doctor for further advice and next steps. For more information about the signs of autism in different age groups, please visit Autism Awareness Australia.